How I Boosted My Immunity Fast During Recovery — Real Talk from My Couch
When I got sick last winter, my energy tanked and I felt stuck. That’s when I realized how crucial immune support is during recovery. I wasn’t looking for miracles—just real, doable steps to feel stronger, faster. After testing small daily changes backed by science, I noticed a real shift. This isn’t a medical fix, but a firsthand look at how smart habits can boost resilience when your body needs it most. What began as a slow, frustrating healing process turned into a powerful lesson in listening to my body, respecting recovery, and making choices that truly supported healing from the inside out.
The Wake-Up Call: When My Body Hit Pause
It started with a persistent cough, then fatigue that no amount of coffee could fix. I had pushed through weeks of busy schedules, skipped meals, and sacrificed sleep, convinced I could power through. But my body had other plans. One morning, I simply couldn’t get out of bed without feeling dizzy and drained. That was the moment I realized I wasn’t just tired—I was healing. The doctor confirmed a viral infection that had weakened my system, and while it wasn’t life-threatening, the recovery phase dragged on longer than I expected. For over two weeks, even simple tasks like folding laundry or walking to the mailbox left me breathless and exhausted.
The emotional toll was just as heavy. I felt isolated, frustrated, and guilty for not being productive. I missed family events, fell behind at work, and struggled with the mental fog that often accompanies prolonged illness. What surprised me most was how much my sense of identity was tied to being active and capable. When that was stripped away, I had to confront a deeper truth: I had taken my health for granted. I had viewed immunity as something that either worked or didn’t—like a switch—but now I saw it as a dynamic system that needed daily support, especially during recovery. This experience became my wake-up call to stop treating my body like a machine that could run indefinitely without maintenance.
What changed wasn’t a sudden cure, but a shift in mindset. Instead of resisting the slowdown, I began to see rest not as failure, but as essential repair work. I stopped measuring my worth by how much I could accomplish in a day and started asking: What does my body need right now? This simple question became the foundation of my recovery journey. It wasn’t about bouncing back to my old pace overnight, but about rebuilding strength in a way that honored the healing process. And slowly, as I adjusted my habits, I began to notice small improvements—more energy by midday, deeper sleep, and a growing sense of calm that I hadn’t felt in years.
Why Immunity Matters Most in Rehab (Not Just Prevention)
Most conversations about immunity focus on staying healthy—avoiding colds, flu, or infections. But what’s often overlooked is how vital the immune system is during recovery. When your body is healing, your immune system isn’t just defending against invaders; it’s actively repairing tissues, reducing inflammation, and reallocating energy to where it’s needed most. This repair mode is just as demanding as fighting off an illness, if not more so. In fact, the immune system consumes significant resources during recovery, which is why fatigue is so common. Without proper support, healing can stall, symptoms may linger, and the risk of secondary infections increases.
One key player in this process is inflammation. In the early stages of illness or injury, inflammation is a natural and necessary response—it helps isolate damage and kickstart healing. But prolonged or uncontrolled inflammation can slow recovery and even contribute to long-term health issues. The immune system’s job is to balance this response: activate when needed, then dial it back once the threat is neutralized. During recovery, this regulation becomes critical. If the body remains in a state of chronic low-grade inflammation, it can impair tissue repair, disrupt sleep, and drain energy reserves. That’s why immune support isn’t just about preventing sickness—it’s about creating the internal conditions that allow the body to heal efficiently.
Another important factor is energy allocation. When you’re sick, your body redirects calories and nutrients away from non-essential functions—like digestion or muscle building—and toward immune activity. This is why appetite often changes during illness and why you may feel weak even after the main symptoms subside. The body is still working behind the scenes, and if you don’t give it the fuel it needs, recovery takes longer. Supporting immunity during rehab means respecting this energy shift—eating nourishing foods, getting quality rest, and avoiding additional stressors that force the immune system to work harder. It’s not about doing more; it’s about doing what truly matters for healing.
The 3 Daily Non-Negotiables That Actually Helped
In the beginning, I was overwhelmed by conflicting advice—take this supplement, try that cleanse, sleep 10 hours, meditate for an hour. I knew I needed simplicity, not more pressure. So I focused on three core habits that research consistently links to immune function: consistent sleep timing, hydration with electrolyte balance, and gentle movement. These weren’t drastic changes, but they made a measurable difference. I didn’t aim for perfection—just consistency. And over time, they became non-negotiables, the foundation of my recovery routine.
First, I prioritized sleep—not just how much, but when. I set a fixed bedtime and wake time, even on weekends. This helped regulate my circadian rhythm, which plays a direct role in immune regulation. Studies show that irregular sleep patterns can suppress immune cell activity and increase inflammation. By going to bed and waking up at the same time each day, I supported my body’s natural repair cycles. I also created a wind-down routine: dimming lights an hour before bed, avoiding screens, and drinking herbal tea. Within a week, I noticed deeper sleep and less brain fog in the morning. Sleep didn’t cure me, but it gave my body the quiet it needed to heal.
Second, I paid attention to hydration—specifically, electrolyte balance. When I was sick, I lost fluids through fever and reduced appetite, and I didn’t realize how much this affected my energy. Plain water helped, but I learned that electrolytes—like sodium, potassium, and magnesium—are essential for cellular function and immune response. I started adding a pinch of sea salt and a squeeze of lemon to warm water in the morning, and I included broth-based soups in my meals. These small changes helped maintain fluid balance, reduce fatigue, and support circulation. I didn’t need fancy drinks—just simple, whole-food sources of minerals. Hydration became less about quantity and more about quality.
Third, I introduced gentle movement. At first, even standing up made me dizzy, so I started with seated stretches and deep breathing. As I gained strength, I added short walks around my living room, then to the porch, and eventually around the block. Movement boosted circulation, which helps immune cells travel through the body more efficiently. It also reduced stiffness and improved my mood. The key was keeping it low-intensity—no pushing, no goals. Just moving enough to wake up my system without overexerting. These three habits—sleep, hydration, and gentle movement—didn’t require special equipment or expensive products. They were accessible, sustainable, and most importantly, effective.
Food Moves I Swapped In (No Superfoods Needed)
I used to think boosting immunity meant eating exotic superfoods or following strict diets. But during recovery, I realized that real support comes from consistent, balanced eating—not perfection. I focused on small, practical food swaps that aligned with what my body could handle. The goal wasn’t to overhaul my diet overnight, but to make choices that nourished my immune system without adding stress.
One of the first changes I made was adding protein to breakfast. On sick days, I often skipped meals or reached for toast and jam, which spiked my blood sugar and left me crashing by mid-morning. I started incorporating soft-cooked eggs, Greek yogurt, or a small portion of nut butter on whole grain toast. Protein helps repair tissues and supports immune cell production. It also keeps you full longer, which matters when your appetite is low. Even a small amount made a difference in my energy levels and reduced afternoon fatigue.
Another shift was increasing the color on my plate. I didn’t aim for a full rainbow every day, but I made a point to include at least two different colored vegetables or fruits in each meal. Red bell peppers, carrots, blueberries, spinach—these foods are rich in antioxidants and phytonutrients that support immune function. I learned that the gut and immune system are closely linked—about 70% of immune cells reside in the gut lining. Eating a variety of plant foods feeds beneficial gut bacteria, which in turn helps regulate immune responses. I didn’t eliminate anything; I just added more color and fiber gradually.
I also reduced processed snacks. When I was tired, it was easy to grab crackers, cookies, or frozen meals. But I noticed that these foods often made me feel more sluggish and bloated. I started replacing them with whole food options: apple slices with almond butter, cucumber rounds with hummus, or a small bowl of oatmeal with cinnamon. These swaps weren’t about restriction—they were about choosing foods that gave me steady energy and supported healing. I didn’t count calories or track macros. I just listened to how my body responded. Over time, my cravings shifted, and I naturally reached for more nourishing options. Food became less of a convenience and more of a healing tool.
Mindset & Rest: The Hidden Immune Boosters
One of the most surprising lessons from my recovery was how much my mental state affected my physical healing. I had assumed that rest meant physical stillness, but I soon realized that mental rest was just as important. Constant worry, self-criticism, and pressure to “get better fast” were silently draining my energy and slowing my progress. I learned that stress triggers the release of cortisol, a hormone that, in excess, can suppress immune function and prolong inflammation. So while I was doing all the right things physically, my mind was working against me.
I started incorporating simple breathwork into my day. Just five minutes of slow, deep breathing—inhaling through the nose, exhaling longer through the mouth—helped calm my nervous system. I did this in the morning and before bed. It wasn’t meditation in the traditional sense, but it gave my mind a break from racing thoughts. Over time, I noticed my heart rate slowed, my sleep improved, and I felt more present. Breathwork became a daily reset, a way to signal to my body that it was safe to heal.
I also learned to set boundaries. I stopped saying yes to every request. I let family know I needed quiet time in the afternoons. I turned off notifications and limited social media. These small acts of protection gave me space to rest without guilt. I also adjusted my expectations. Instead of measuring progress by how much I could do, I celebrated small wins—sitting up for 20 minutes, cooking a simple meal, laughing with a friend. This shift in mindset reduced pressure and allowed me to be kinder to myself. Healing isn’t linear, and progress isn’t always visible. But by honoring my limits and prioritizing mental rest, I created the internal conditions for my immune system to function more efficiently.
What My Doctor Actually Recommended (And What I Added)
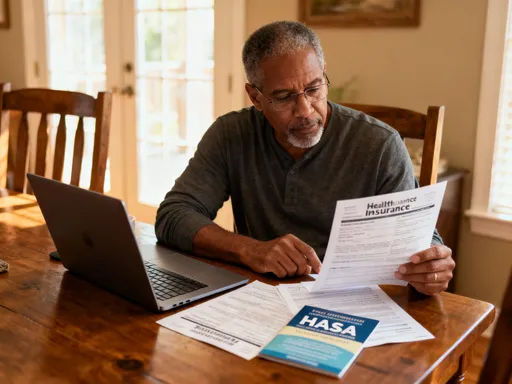
Throughout my recovery, I stayed in close contact with my doctor. Their advice was grounded, practical, and focused on evidence-based care. They emphasized rest, monitoring symptoms, and following up if anything worsened. They didn’t push supplements or extreme diets—just clear guidance on what my body needed at each stage. One of the most reassuring things they said was: “Healing takes time. There’s no shortcut, but there are ways to support the process.” That gave me permission to slow down without feeling like I was failing.
My doctor also reminded me that immunity isn’t something you boost overnight. It’s influenced by long-term habits—sleep, nutrition, stress management, and physical activity. They supported my focus on hydration and gentle movement but cautioned against overexertion. They also reviewed my medications and ensured I wasn’t taking anything that could interfere with healing. This collaboration was crucial. I didn’t see lifestyle changes as a replacement for medical care, but as a complement. I followed their guidance while adding small, personalized habits that worked for my daily life.
What I added—like breathwork, food swaps, and structured rest—weren’t medical treatments, but they enhanced my overall well-being. I kept a journal to track how I felt each day, which helped me identify patterns. For example, I noticed that days with better sleep and less screen time correlated with improved energy. Sharing these observations with my doctor helped us make informed decisions together. This partnership—between professional care and personal responsibility—was key to my recovery. It wasn’t about choosing one over the other, but integrating both to support healing in a balanced, sustainable way.
Building a Recovery-Ready Routine That Sticks
As I regained strength, I faced a new challenge: how to maintain these habits beyond recovery. I didn’t want to fall back into old patterns once I felt better. So I focused on habit stacking—linking new behaviors to existing routines. For example, I paired hydration with my morning tea ritual, and I attached gentle stretching to checking the weather each day. These small anchors made the habits easier to remember and sustain. I also embraced the idea of small wins. Instead of aiming for an hour of movement, I celebrated five minutes. Instead of perfect meals, I focused on one nourishing choice at a time. Progress wasn’t measured by speed, but by consistency.
I also learned to listen to my body’s signals. Some days, I had more energy and could walk farther. Other days, I needed extra rest. I stopped judging myself and started responding with care. This awareness helped me avoid burnout and stay in tune with my needs. I created a simple weekly plan—nothing rigid, just a loose framework that included sleep goals, meal ideas, and rest periods. I kept it visible on my fridge, not as a to-do list, but as a gentle reminder of what supported my health.
Most importantly, I began to view recovery not as an interruption, but as a phase of growth. The habits I built during illness became part of my long-term lifestyle. I still prioritize sleep, eat colorful meals, and take mental breaks when needed. I no longer see these as “recovery tools,” but as everyday practices that support resilience. Healing taught me that strength isn’t just about endurance—it’s about balance, patience, and self-awareness. By treating recovery as a proactive health phase, I gained more than just energy. I gained a deeper respect for my body and a commitment to honoring its needs, not just when I’m sick, but every day.
Looking back, I wouldn’t wish that winter illness on anyone. But I’m grateful for what it taught me. Boosting immunity during recovery isn’t about quick fixes or miracle cures. It’s about making thoughtful, consistent choices that support your body’s natural ability to heal. It’s about rest, nourishment, movement, and mindset—all working together. And while the journey was slow, it was also transformative. I emerged not just stronger, but wiser. I learned to trust the process, to value rest, and to treat my body with the care it deserves. If you’re in recovery now, know this: healing is not a race. It’s a quiet, powerful act of self-respect. And every small step you take to support it matters.